Myeloma cast nephropathy

76 year old female presenting with a slowly enlarging mass
November 3, 2019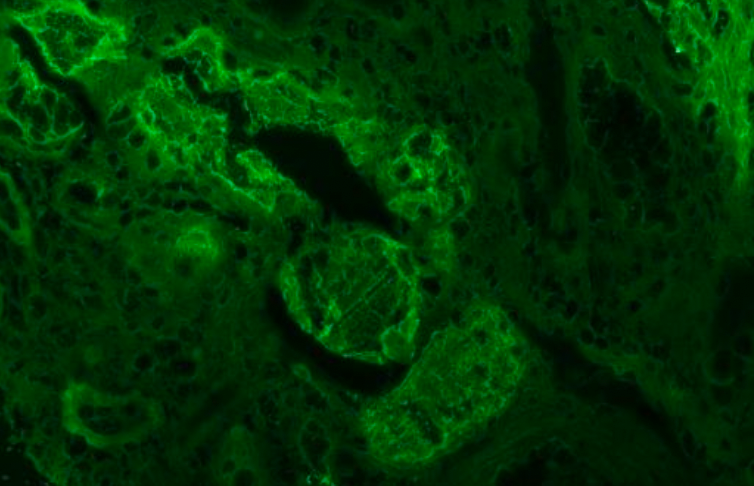
Case submitted By Dr. Abeer Altahrawi (resident), Diagnosed and signed out by Dr. Stephan Ward, Attending pathologist, Mount Sinai Health System.
Case
A 58-year old woman with no known past medical history, presented with nausea, vomiting and diarrhea for 3 weeks after a recent trip to South America. Persistent nausea and vomiting led to limited oral intake. She had no history of hematemesis, blood, melena or mucous in her stool. She also described pain and weakness in her lower limbs while walking. Three days prior to presentation, her weakness progressed to the point where she needed a wheelchair. She also noticed abdominal distension and started to have decreased urine output.
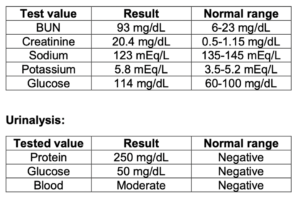
Her initial evaluation at the emergency department was remarkable for high blood pressure (BP: 163/83) and the following lab results:
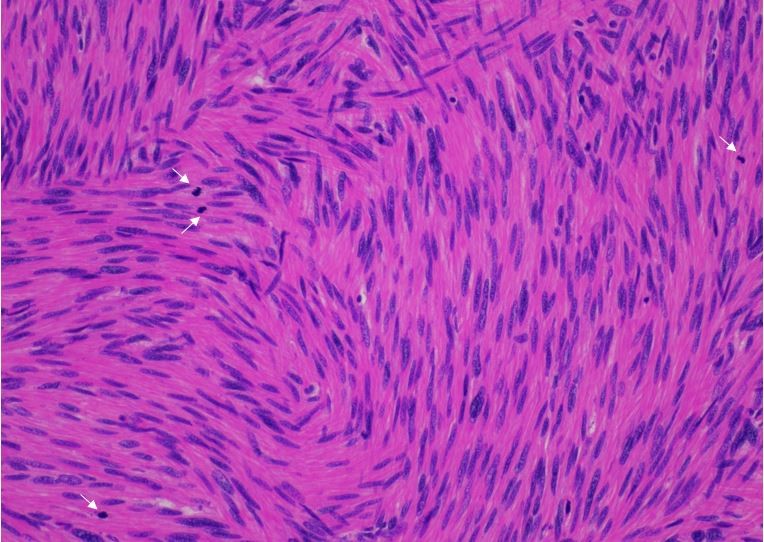
A renal biopsy was performed.
Microscopic examination revealed fractured intratubular casts (shattered glass appearance), surrounded by giant cells and causing tubular rupture in some sections. This was associated with lymphoplasmacytic interstitial inflammation and moderate parenchymal fibrosis. The glomeruli appeared within normal limits. The relevant casts appeared pale and glassy on PAS and had a metachromatic appearance on Masson trichrome stain. Immunohistochemical and Immunofluorescence stains for kappa and lambda showed those casts to be lambda restricted. Congo red stain was negative. Both electron microscopy and immunofluorescence were negative for glomerular immune complex deposition. A diagnosis of myeloma cast nephropathy was made.
The patient then underwent a bone marrow biopsy and aspirate that showed CD138-positive, lambda restricted plasma cells involving 50-60% of the marrow cellularity, leading to a diagnosis of multiple myeloma. Multiple myeloma is a plasma cell proliferative disorder that commonly involves the kidney. Renal impairment is a serious complication that is associated with a higher tumor burden and increases mortality and, morbidity (1).
Discussion
Intratubular casts are frequently seen on kidney biopsies and can be part of normal renal physiology, a result of glomerulonephritis (e.g. red blood cell casts) or as a consequence of systemic disease (2).
Hyaline casts are the most commonly encountered type of casts in renal biopsies. They are defined as uniformly staining, pale-pink rounded structures, filling the lumina of the loop of Henle and the distal tubule. They are often associated with thyroidization-type tubular atrophy and can be intermixed with inflammatory cells, including neutrophils and lymphocytes (2).
While uromodulin is one component of hyaline casts, uromodulin casts are formed entirely of this protein. Uromodulin is the most abundant protein found in normal urine and it protects the urothelium against infections. Uromodulin casts are characterized by a frothy appearance on light microscopy and stains strongly positive for PAS, helping in differentiating them from the pathologic myeloma casts (2).
Light chains are constantly produced by the lymphoid system and these proteins are generally re-absorbed by the proximal tubular epithelial cells. In plasma cell dyscrasias, light chains are produced in large amounts, exceeding the capacity of re-absorption by tubular epithelial cells (2) and leading to the formation of light chain casts. Light chain casts are typically present in distal nephron segments, although they can be seen within the proximal tubules & rarely within Bowman’s space. They are typically pale on PAS and appear glassy & homogenous, while they are metachromatic on Masson trichrome stain. Fracture lines are often seen and casts may protrude beyond the limit of the biopsy core. A giant cell reaction is helpful, but neither sensitive nor specific. Rarely, myeloma casts can be positive for Congo red stain. A diagnosis of myeloma cast nephropathy can be made when these histologic features are combined with evidence of light chain restriction (2). Light chain cast deposition is often associated with tubular atrophy and interstitial inflammation, which might make the term myeloma kidney more appropriate than cast nephropathy (3).
Figure 1: A. Fractured intratubular casts (shattered glass appearance), surrounded by giant cell reaction (H&E stain). B. The same casts stain pale with the PAS stain. Immunohistochemistry for kappa and lambda shows lambda restriction.
Figure 2: Immunofluorescence for Kappa and Lambda showing Lambda restriction in the relevant intratubular casts.
References:
- Sathick IJ, Drosou ME, Leung N. Myeloma light chain cast nephropathy, a review. J Nephrol. 2019 Apr;32(2):189-198. doi: 10.1007/s40620-018-0492-4. Epub 2018 May 5. PMID: 29730782.
- Dvanajscak Z, Cossey LN, Larsen CP. A practical approach to the pathology of renal intratubular casts. Semin Diagn Pathol. 2020 May;37(3):127-134. doi: 10.1053/j.semdp.2020.02.001. Epub 2020 Feb 14. PMID: 32147230.
- Sanders PW. Mechanisms of light chain injury along the tubular nephron. J Am Soc Nephrol. 2012 Nov;23(11):1777-81. doi: 10.1681/ASN.2012040388. Epub 2012 Sep 20. PMID: 22997259.