President’s Symposium Handouts
May 3, 2018Viral Associated Neoplasms of Head and Neck – Presentation Material
September 23, 2018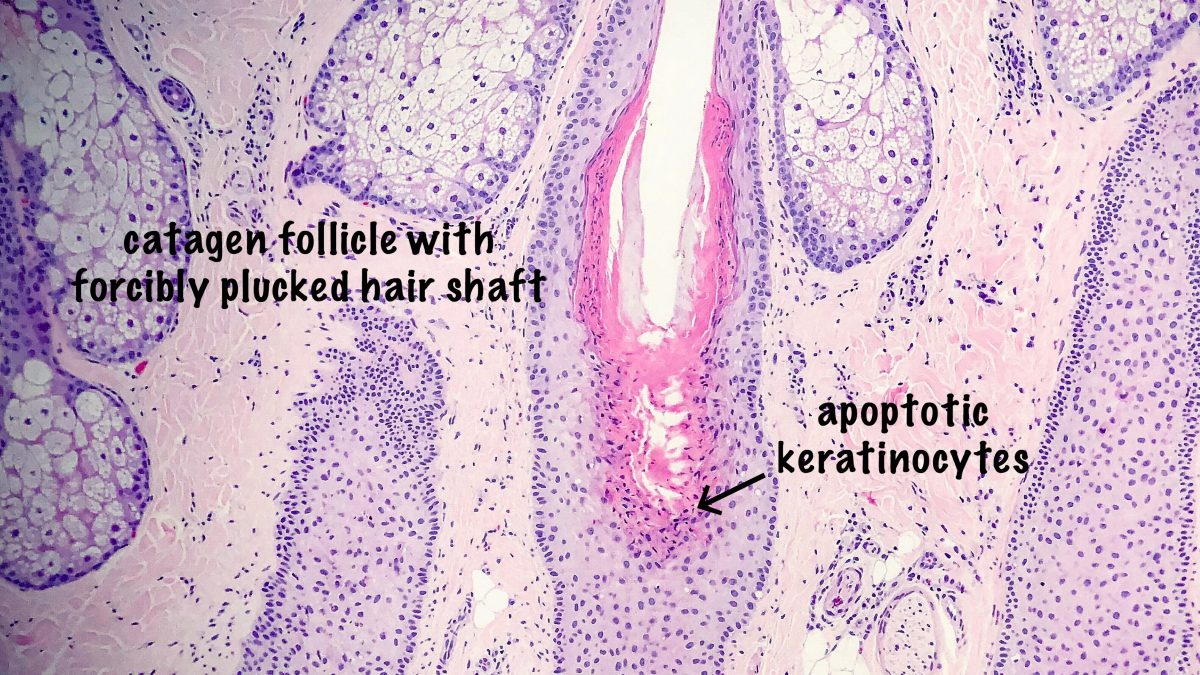
Trichotillomania is a rare form of non-scarring alopecia, mainly on the scalp, sometimes the eyebrows, which occurs as a result of conscious or unconscious, frequent hair pulling in patients that experience a significant amount of psychological stress. Clinically, the alopecic patches show bizarre, geometric shapes with retention of short hair follicles. Trichotillomania can be seen in children and in adults; while some series show a female predominance, others show no gender predilection.
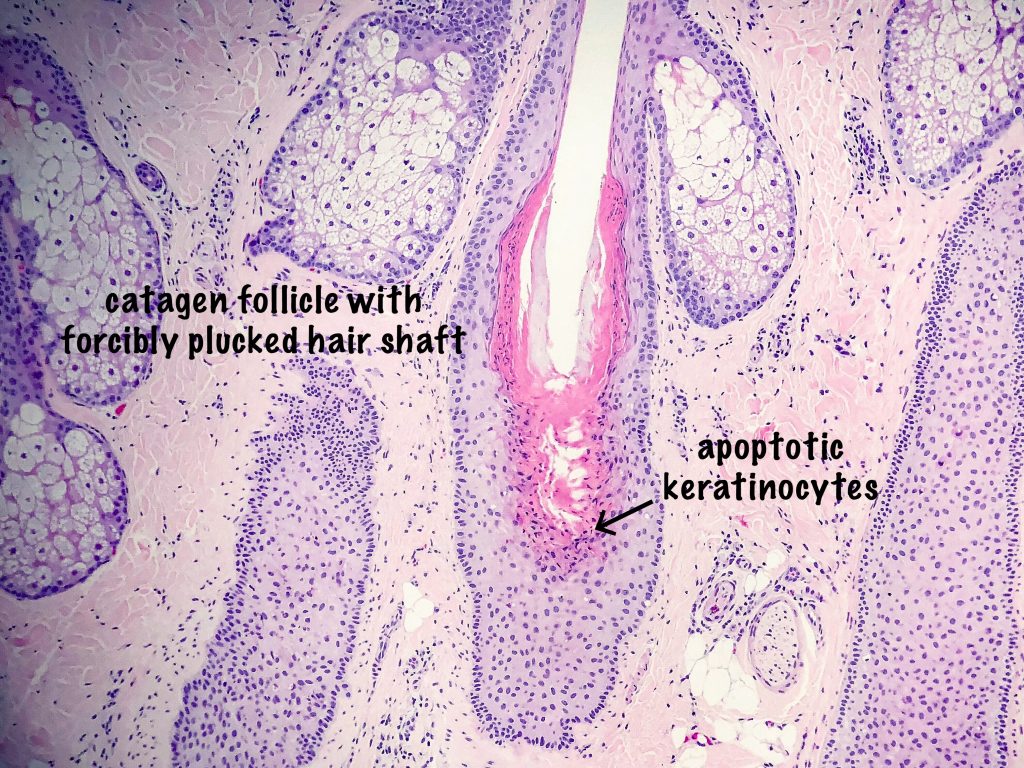
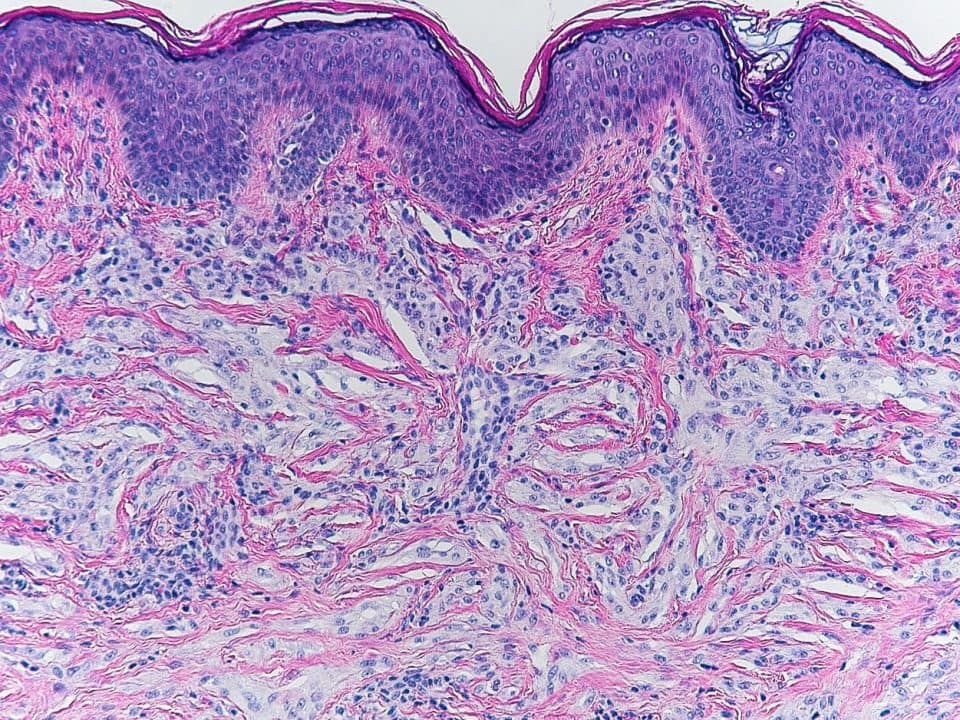
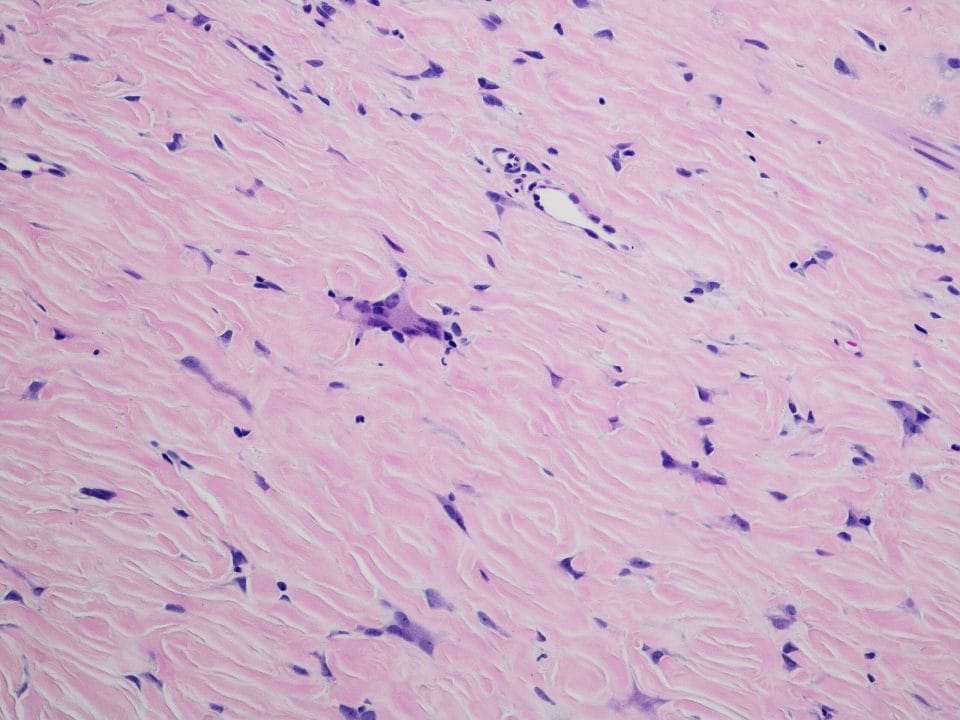
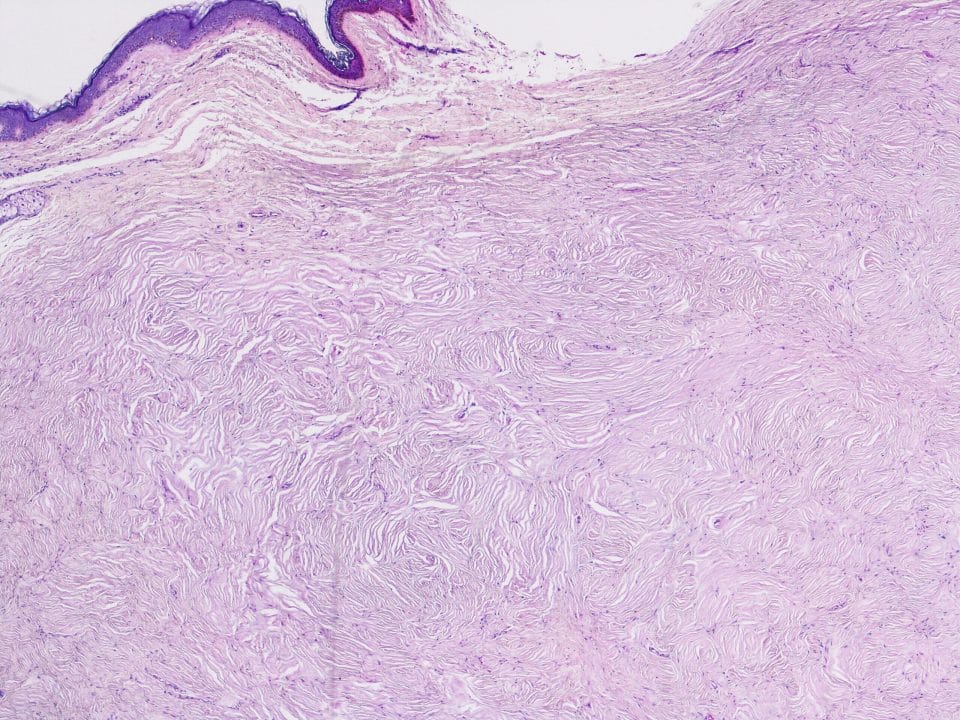
Histologic findings reveal a pauci-inflammatory, non-scarring alopecia with increased catagen and telogen count. Catagen hair follicles are easily distinguished by the presence of scattered apoptotic keratinocytes in the follicular epithelium. Here, it is the mechanical trauma that is responsible for the early transition of anagen phase to catagen phase. The telogen phase tends to follow the catagen phase several weeks after the mechanical trauma has passed.
Notable histologic findings of trichotillomania are the following:
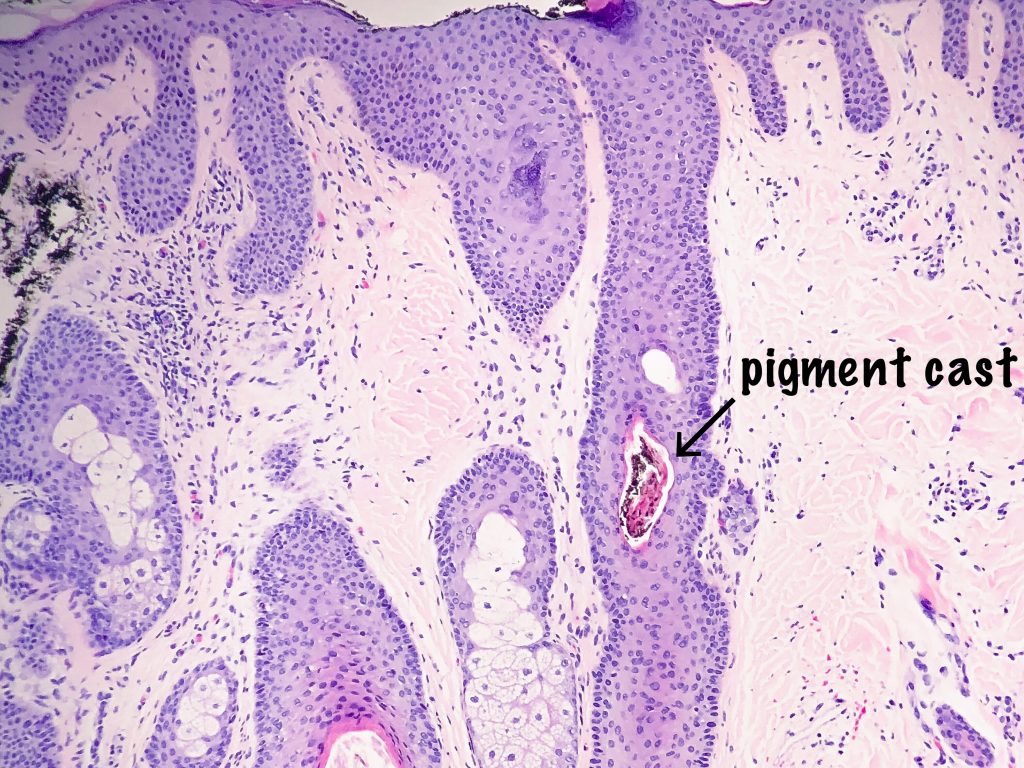
- Pigment hair casts – ectopic pigmented matrix cells which contain melanin. Once these cells become stranded in the follicular epithelium above, they decrease in size, cornify and become the well recognizable pigmented hair cast.
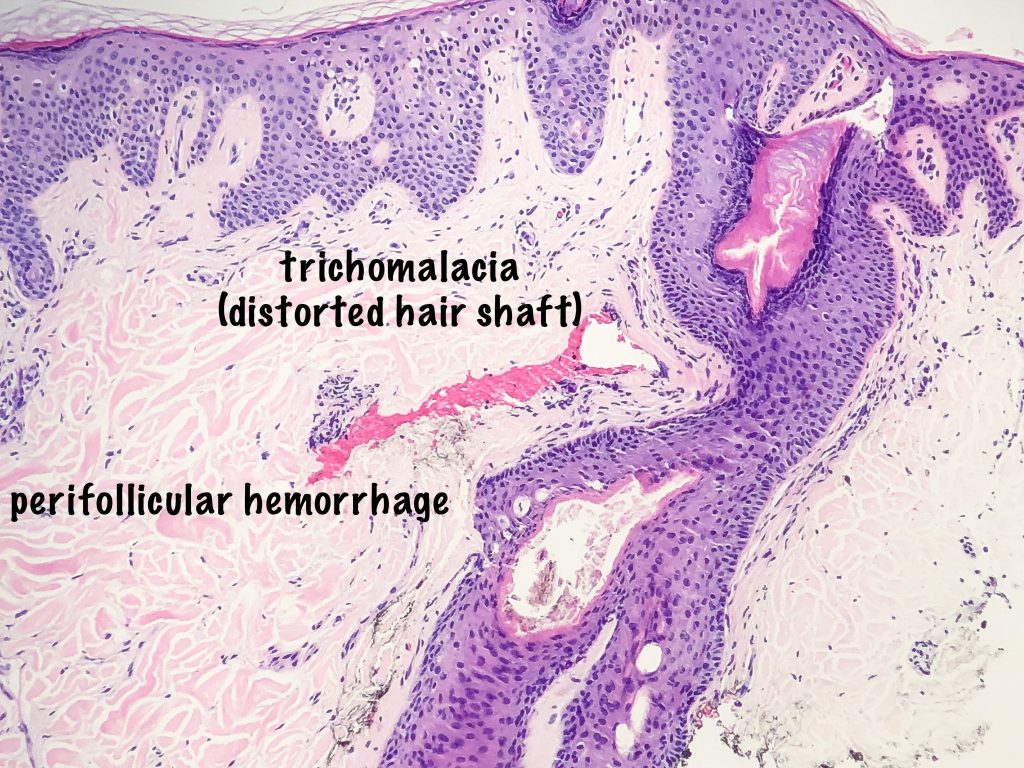
- Trichomalacia – distorted hair shaft, these can be numerous.
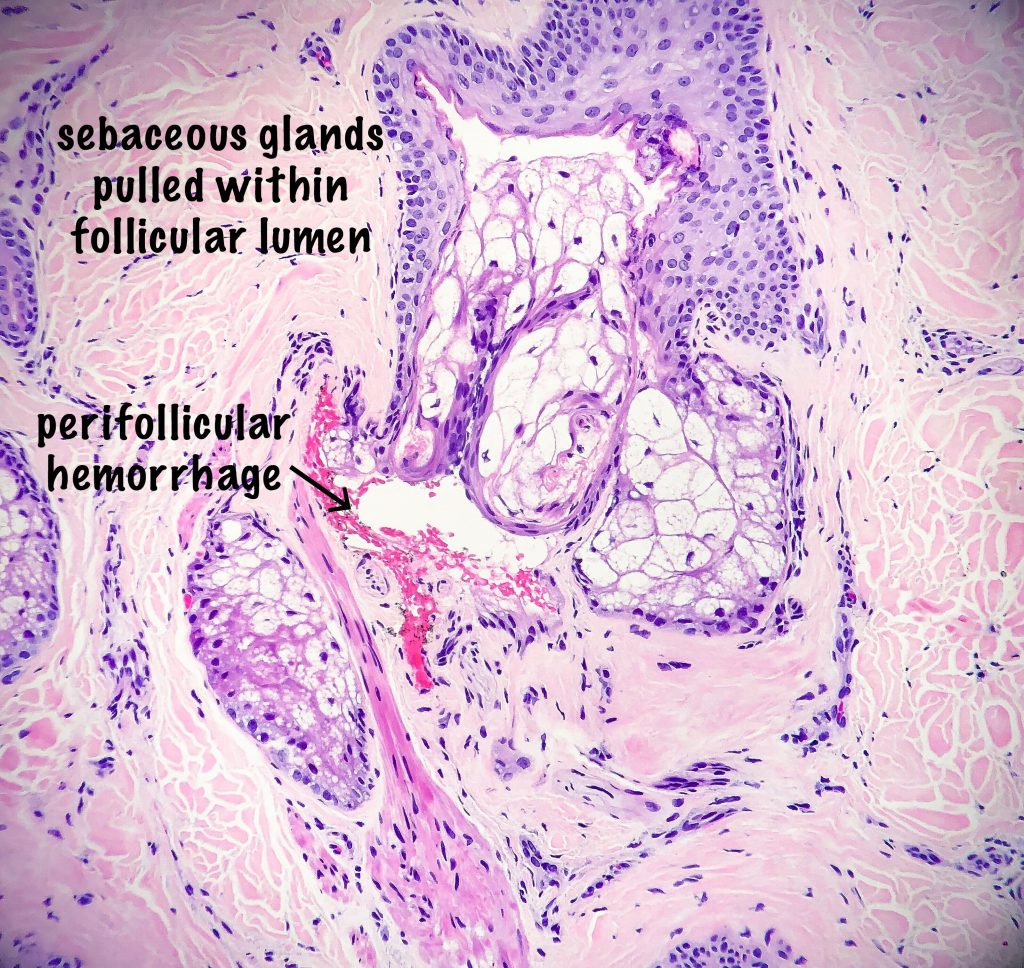
- Perifollicular and intrafollicular hemorrhage – extravasated red blood cells can also be present.
- Displaced sebaceous glands – notably sebaceous glands can be pulled within the follicular lumen secondary to the mechanical trauma.
- On horizontal sections, sometimes fractured hair shafts can be seen with fibrin and extravasated red blood cells between the two halves of the hair shaft. This has been called “the hamburger sign.” For good examples of this finding, please visit the following link: https://goo.gl/images/9EFBQM, and reference #3 below.
In the end, after the pathologist makes the diagnosis of trichotillomania, the hardest part of the journey has yet to begin. This is the part where the clinician supports the patient to a road of wellness. Some authors have suggested that trichotillomania should be replaced with the term “neuro-mechanical alopecia,” and I agree with this patient-centered nomenclature.
As always, thank you for taking the time to visit the monthly dermatopathology blog,
Kind regards,
Silvija P. Gottesman, MD, FAAD
Dermatologist/Dermatopathologist
Assistant Professor of Dermatology and Pathology
Zucker School of Medicine at Hofstra/Northwell
Twitter: @SGottesmanMD
Further Reading:
- Sperling, Leonard C., et al. An Atlas of Hair Pathology with Clinical Correlations. Trichotillomania. Informa Healthcare, 2012.
- Bergfeld W, Mulinari-Brenner F, McCarron K, et al. The combined utilization of clinical and histological findings in the diagnosis of trichotillomania. J Cutan Pathol 2002;29:207–214.
- Royer MC, Sperling LC. Splitting hairs: The ‘hamburger sign’ in trichotillomania. J Cutan Pathol 2006;33(Suppl. 2):63–64.
- Walling HW, Swick BL. Psychocutaneous syndromes: A call for revised nomenclature. Clin Exp Dermatol 2007;32:317–319.