NYPS President’s Symposium
March 31, 2018President’s Symposium Handouts
May 3, 2018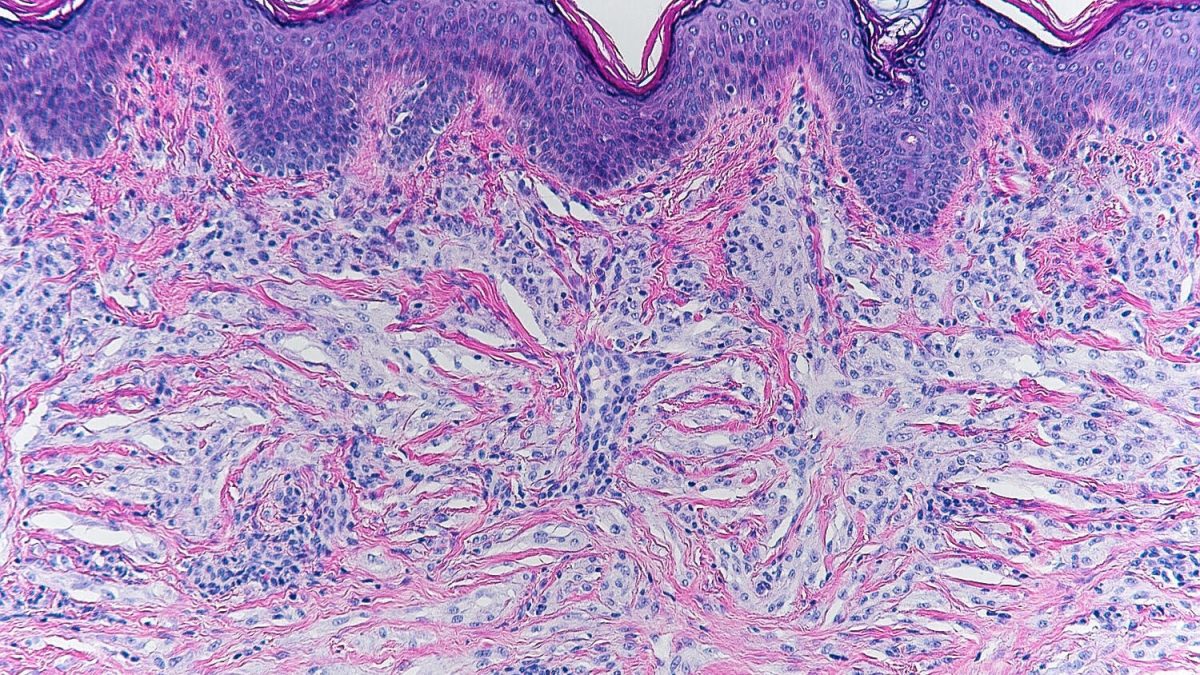
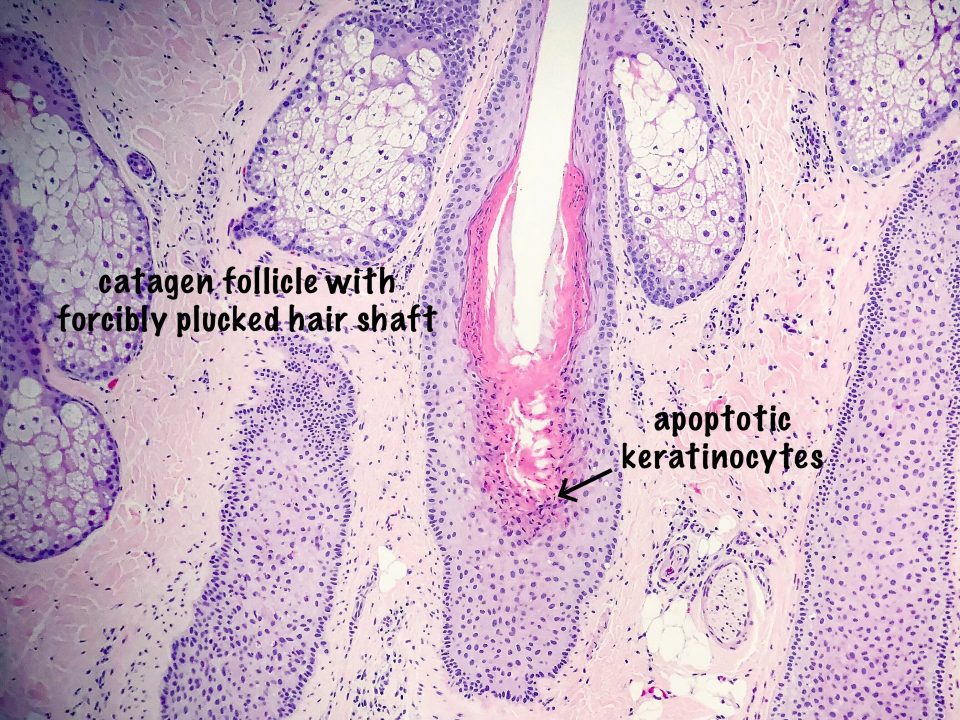
A 5-month-old female patient was brought to the dermatology clinic for evaluation of a 0.7cm reddish-brown, mobile nodule located on the left upper flank. The lesion was asymptomatic and over the course of 7 months, a slow growth was noted. At 12 months of age, the lesion had reached 1.2cm in size and was biopsied.
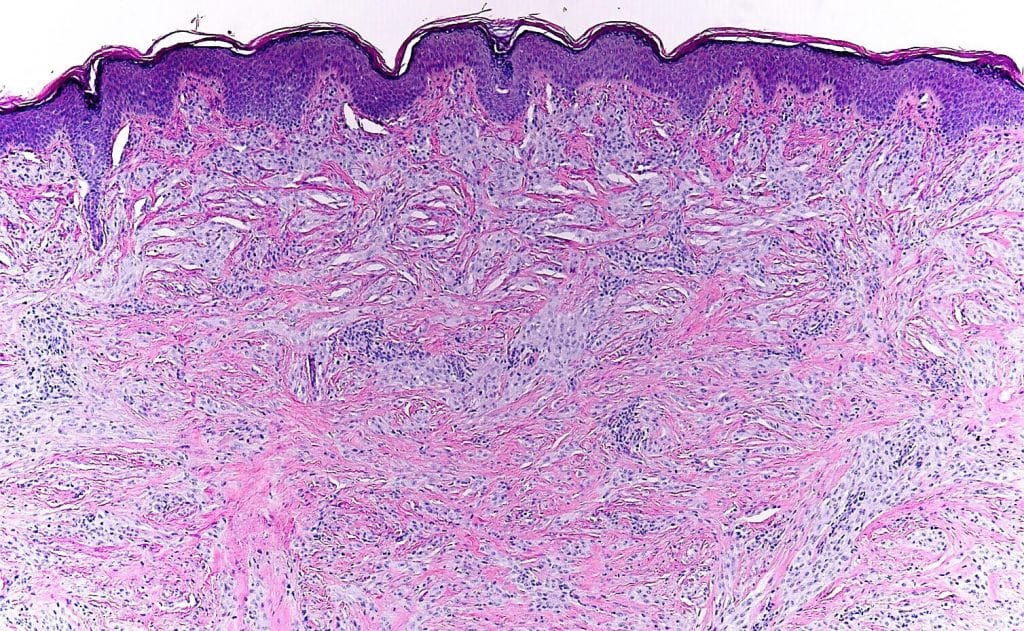
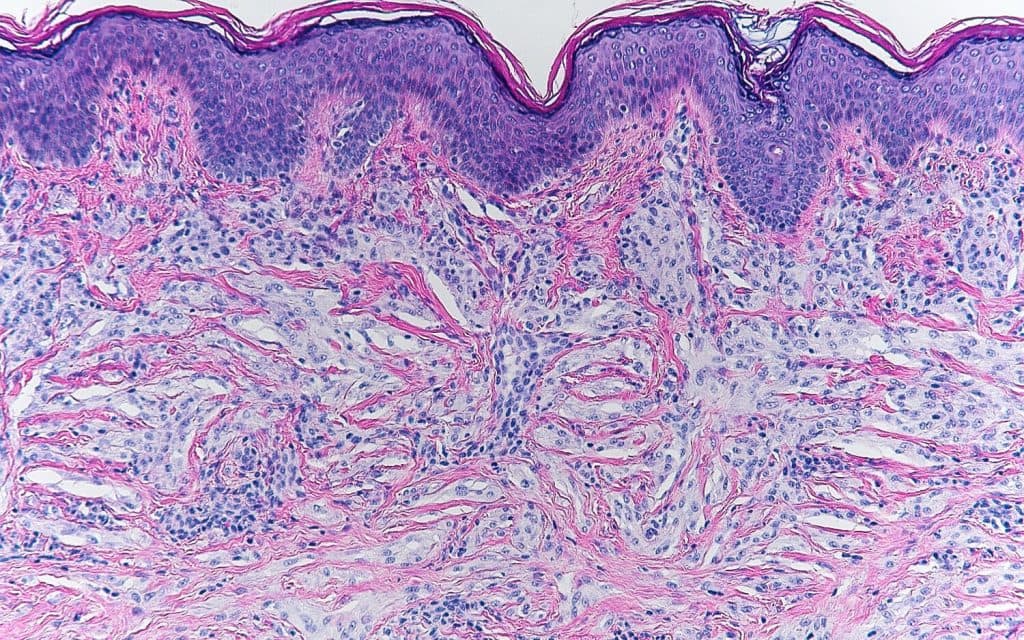
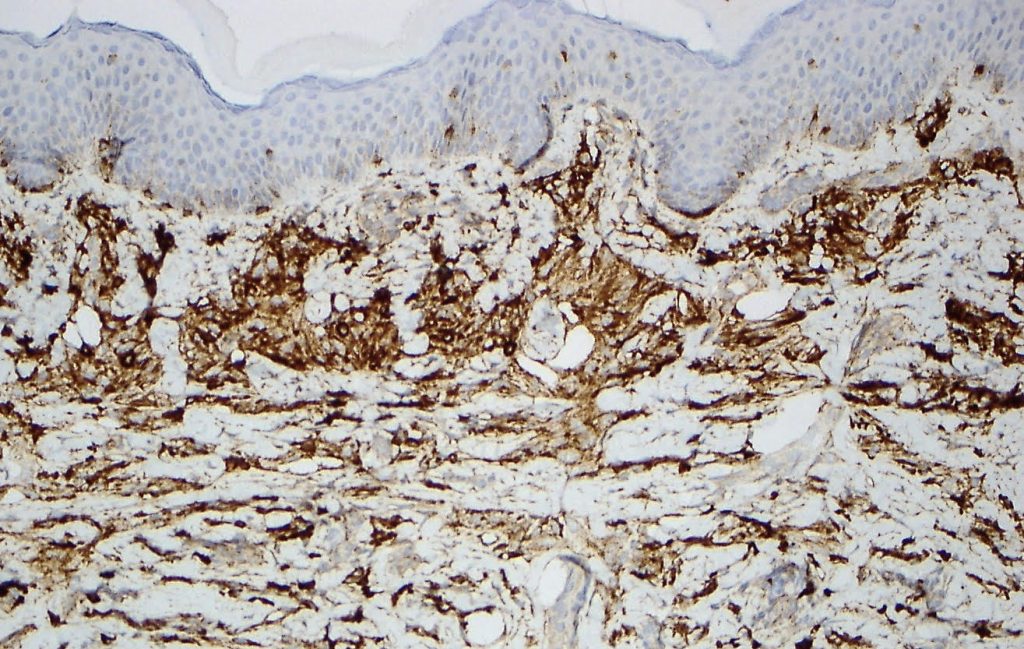
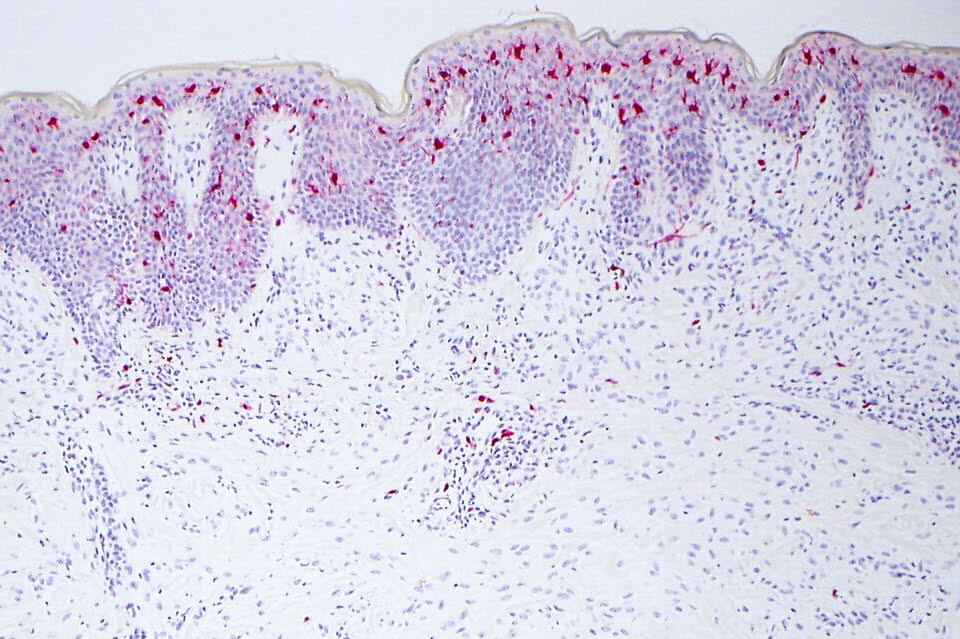
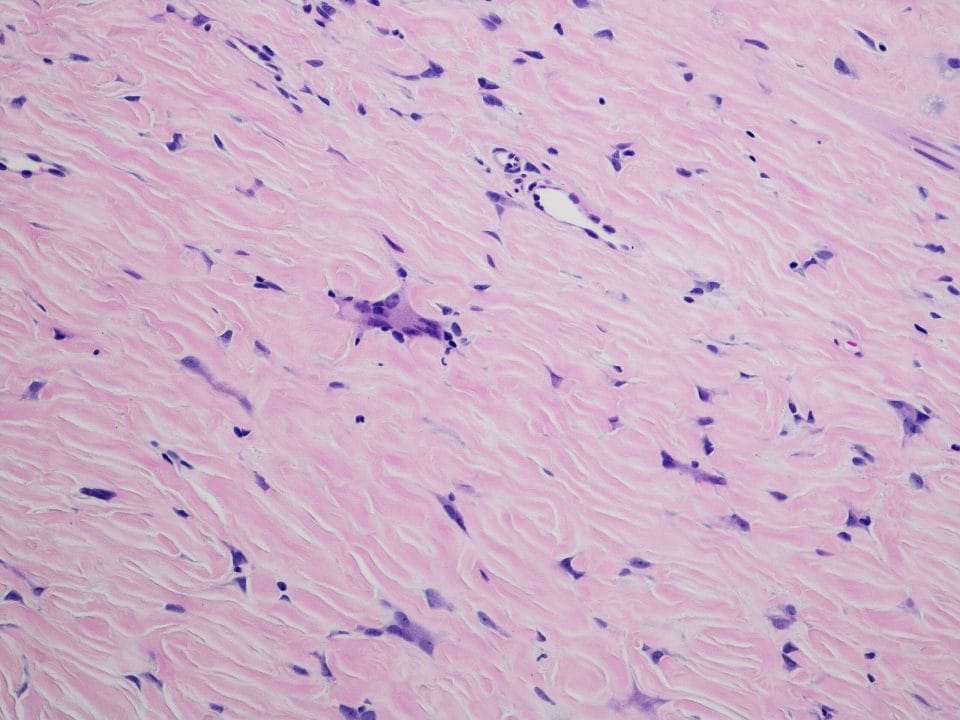
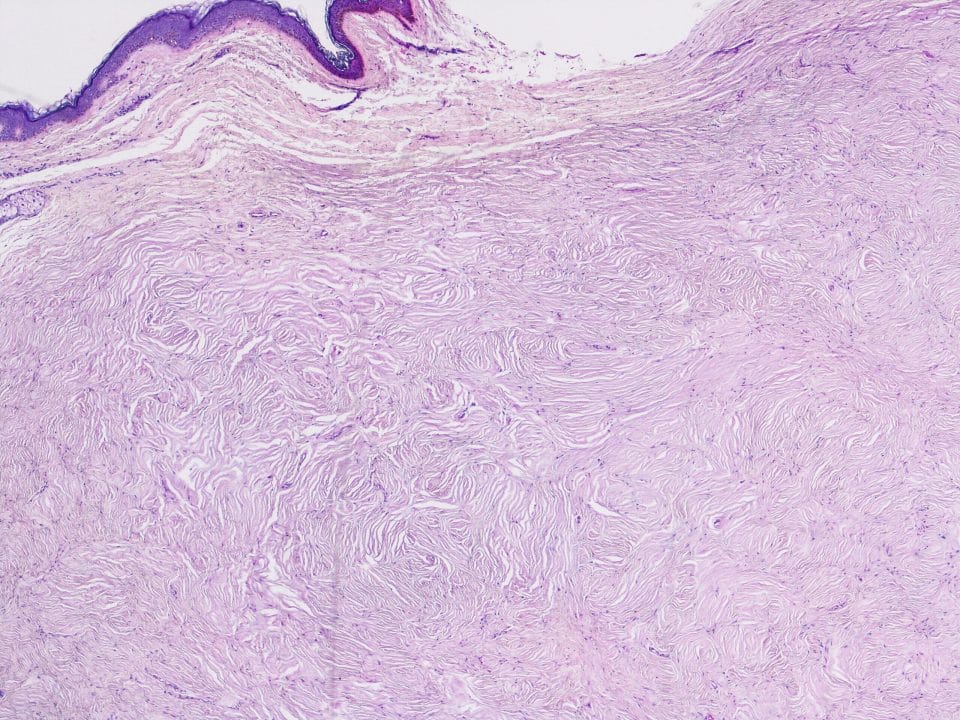
Hematoxylin and eosin (H&E) stained sections show absence of an epidermal component and a dermal infiltrate of rounded and fascicular collections of uniform cells with lightly amphophilic cytoplasm. These uniform cells have enlarged vesicular nuclei and the collections are surrounded by a fibrotic stroma. Immunohistochemistry (IHC) analysis of the neoplasm showed diffuse cytoplasmic staining with NKI/C3. Stains for CD163, Melan-A, and S-100 protein were negative, excluding the diagnosis of melanoma, Spitz nevus and cutaneous histiocytoma. On high power, there was no evidence of any foamy histiocytes or Touton giant cells, excluding a diagnosis of juvenile xanthogranuloma as well. Given the H&E and IHC findings, the diagnosis is cellular neurothekeoma.
Figure 1: There is a poorly circumscribed dermal infiltrate of rounded and fascicular collections of uniform cells (H&E, x100 magnification).
Figure 2: These uniform cells have lightly amphophilic cytoplasm and are surrounded by a fibrotic stroma (H&E, x200 magnification).
Figure 3: The cells show diffuse cytoplasmic staining (NK1/C3, x200 magnification).
Figure 4: The lesional stains fail to stain with S100 immuno stain. Of note, positive internal control is seen; Langerhans cells in the stratum spinosum are nicely highlighted (S100, x100 magnification).
Neurothekeomas were first described under the name of nerve sheath myxoma and their classification was based on different histologic appearance and is divided as follows: classic (also known as myxoid or hypocellular), cellular, and mixed type (1,5). The classic type has a lobulated growth pattern and has an abundant myxoid stroma. It typically stains positively for S-100 protein. Conversely, the cellular type appears as bundles of epithelioid and spindle cell nests with prominent amphophilic cytoplasm. It does not stain positively for S-100 protein and consistently stains positively for NKI/C3 (1,2,3).
In 2005, it was postulated that these two entities, neurothekeoma and cellular neurothekeoma likely have different origins (5). Neurothekeoma is also known as dermal nerve sheath myxoma, whereas cellular neurothekeoma is now thought to have a fibrohistiocytic origin thus accounting for the difference in the immunohistochemistry profile (5). Cellular neurothekeoma does not possess a distinct and identifying clinical presentation compared to some other dermal tumors, which is why biopsy with subsequent histopathologic and immunohistochemistry analysis is necessary for definitive diagnosis of this entity. The differential diagnosis, based on similar histologic features, includes fibrohistiocytic, neural, and melanocytic lesions, including dermal Spitz nevi and desmoplastic melanoma (4). Given that NKI/C3 has been shown to positively stain juvenile xanthogranuloma, atypical fibroxanthoma, cellular fibrous histiocytoma, Spitz nevus, and melanoma, is not specific for cellular neurothekeoma, and a diagnosis should not be rendered based on the sole positivity of this marker without appropriate corresponding negative findings in the immunophenotype and histopathologic pattern (3,5). Fortunately, cellular neurothekeoma is consistently negative for S-100, Melan-A, and HMB-45 (4,5).
Cellular neurothekeoma is a benign cutaneous dermal neoplasm that most frequently occurs on the head, neck, or upper trunk of children and young adults. These lesions are often described as slow-growing and asymptomatic (3,6). Several dermal tumors clinically have appearance similar to that of cellular neurothekeoma, i.e. flesh colored asymptomatic nodules. These tumors include juvenile xanthogranuloma, cutaneous lymphoma, Spitz nevus, malignant melanoma, leiomyoma, neurofibroma, pilomatricoma, and dermoid cyst. Only a biopsy would lead to a definitive diagnosis. Cellular neurothekeoma is rarely described in infants; however, it should be considered in the differential diagnosis for dermal tumors that present in this age group.
Special thanks to Drs. Brittany Grady and Geoffrey Gottlieb for their contribution in preparation of this write up.
Hope you join me next month for another brief but exciting and educational dermatopathology article,
Kind regards,
Silvija P. Gottesman, MD, FAAD
Dermatologist/Dermatopathologist
Assistant Professor of Dermatology and Pathology
Zucker School of Medicine at Hofstra/Northwell
Twitter: @SGottesmanMD
References:
- Papadopoulos EJ, Cohen PR, Hebert AA. Neurothekeoma: report of a case in an infant and review of the literature. JAAD 2004; 50(1): 129-134.
- Barnhill RL, Dickersin GR, Nickeleit V, et al. Studies on the cellular origin of neurothekeoma: Clinical, light microscopic, immunohistochemical, and ultrastructural observations. JAAD 1991; 25(1): 80-88.
- Pan H, Tseng S, Weng, C, Chen Y. Cellular neurothekeoma of the upper lip in an infant. Pediatr Neonatol 2014; 55(1): 71-74.
- Gray ME, Palileo CM, Sheridan RM. Cellular neurothekeoma of the eyelid in a 6-year-old boy. J AAPOS 2016; 20(4): 374-376.
- Stratton J, Billings SD. Cellular neurothekeoma: analysis of 37 cases emphasizing atypical histologic features. Mod Pathol 2014; 27(5): 701-710.
- Yarbrough K, Krol A. Cellular neurothekeoma: a review of two pediatric cases. JAAD 2015; 72(5): AB104.